Blood oxygen can’t get up all the time … The five words of the director are true.
Original Bai Ding Medical Respiratory Channel
* For medical professionals only.

Who is in the hands of this case may be a hot potato!
Walking by the river often will definitely wet your shoes.
The case I encountered really made me "wet my shoes".
According to the hospital practice, there are always several working days in the afternoon every week, and I have to attend the preoperative case discussion in several departments like a star.
This is a joint case.
The patient was transferred from Xiabian County Hospital. His age is not too big. He is about 40 years old, but he has been in bed for three years because of nasopharyngeal carcinoma and cerebral infarction.
Because of the femoral neck fracture, I had a femoral head replacement in the county hospital, and the femoral head slipped out after the operation. Ask a superior hospital expert for a second operation, and the result is prolapse again.
The patient’s wife, a salesman of an insurance company, has claimed compensation from the local county hospital for more than two months. Seeing that the Spring Festival was coming, the county hospital was going to celebrate the Spring Festival, so they transferred the patients to our side through the relationship.
The focus of case discussion is surgical indications and surgical risks.
The director of the joint department is a well-known expert in the military, and he has a very clear grasp of the indications for the operation: the tension of the constrictors in the thigh of the patient after cerebral infarction is obviously increased, which will inevitably lead to the prolapse of the femoral head after surgery, which is a contraindication for femoral head replacement, that is to say, the local county hospital has done an operation that should not be done.
The problem we need to solve is to relieve the pain caused by femoral head prolapse. The operation is very simple, just take out the implanted femoral head. After the operation, it is natural to send it to the intensive care unit (ICU) for monitoring. I asked my family members about their medical history in detail. Due to cerebral infarction, the patients could not take care of themselves before operation, so they could only eat some liquid food.
I particularly emphasized the problem of avoiding choking and aspiration after operation, and finally said: "This patient is a hot potato, and there have been medical disputes outside the hospital, so we have to be careful. Whoever falls on the hand burns who. "
Who knows, in a word, this sweet potato finally burned my hand.
The operation was very smooth, and the patient was sent to ICU as scheduled after the operation, with clear consciousness and stable vital signs. Because of the combined spinal-epidural anesthesia, the pillow was removed and the routine rehydration monitoring was performed after operation.
If there is no accident, I will be fine when I return to the orthopedic ward the next morning.
At 6:00 the next morning, my mobile phone rang, and it was the doctor on duty: "Director, come here too soon, bed 3 can’t breathe well!" "
Damn it! Bed 3, the hot potato, made my head grow big.
When I rushed to the department, the patient breathed more than 30 times per minute, and the pulse oxygen saturation dropped to 72%. The chest radiograph beside the emergency bed almost turned white in the whole right lung (Figure 1).
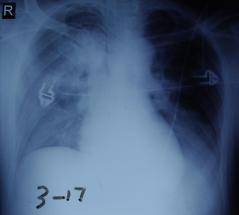
figure 1
Emergency tracheal intubation, ventilator support, the patient’s oxygen saturation gradually rose to 90%.
With a sigh of relief, I asked the reason of the problem in some flustered and frustratedly. The nurses on duty made it clear that the patient had been breathing smoothly before, without vomiting, and no vomit was found beside the bed. Looking back at the monitoring information, the patient did breathe smoothly before 6: 00, and the oxygen saturation was always 97%-100%.
Considering that the possibility of aspiration cannot be ruled out, I decided to have a fiberoptic bronchoscopy immediately.
Bronchial congestion and edema at all levels of the right lung, and no obvious food residue was seen.
In the absence of local anesthesia, the patient did not have obvious cough during awake tracheal intubation and fiberoptic bronchoscopy. I guess the patient’s cough reflex was weakened due to pseudobulbar paralysis of cerebral infarction, and gastric acid reflux and aspiration after operation led to aspiration pneumonia and respiratory failure.
So we used dexamethasone 5 mg to add normal saline to do right lung lavage while breathing support. At the same time, low-dose methylprednisolone 80 mg was given intravenously for 3 days, and antibiotics were used preventively to control lung infection.
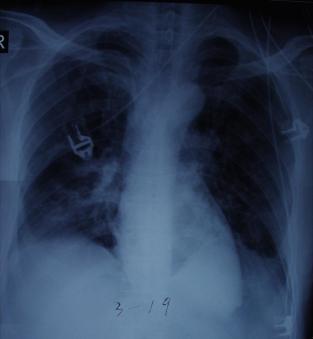
Figure 2
Two days later, the patient’s breathing condition improved obviously, and the right lung exudation was basically absorbed by the chest X-ray (Figure 2).
Just when everyone thought that they could go offline soon, the patient gradually developed severe breathing difficulties at around 16: 00 on the seventh day, and the support conditions of the ventilator were greatly increased, which had no effect at all. Even if pure oxygen was inhaled, the oxygen saturation could only be barely maintained at about 80%.
After trying to use various antiasthmatic and anti-inflammatory drugs, the patient finally saw a turn for the better at about 6: 00 the next morning, and the oxygen saturation gradually rose to 90%, and the number of breaths was not so urgent.
Everything seems to be returning to the good direction all morning, and the ventilator parameters can gradually drop to an acceptable range. Who knows that in the afternoon, at about the same time, like a weird "alarm clock" ringing, the same situation happened again.
Another night of rescue lasted until dawn.
On the third day, the "alarm clock" still arrived on time.
In the face of the accusations and doubts of patients’ families and the frustration and frustration of the team, I tried to dismantle this magic "alarm clock" for three days in a row.
Compared with a stack of doctor’s orders and special care sheets, I finally found some clues in a rotten hemp: fat emulsion injection!
On the seventh day, the doctor added 20% fat emulsion 250 mL intravenous drip qd because of the poor nutritional status of the patient and insufficient heat of nasal feeding liquid.
The execution time of fat emulsion basically starts around 12: 00 noon, and it takes about 3 hours, that is, it is completed around 15: 00. About 1 hour after fat emulsion infusion, the patient’s respiratory condition gradually deteriorated.
According to the instructions, the intravenous drip speed of fat emulsion is required to be no less than 4 hours, and our drip speed obviously exceeds the instructions. One of the adverse reactions of fat emulsion is respiratory symptoms, which is a bit like fat embolism syndrome after fracture. With the idea of giving it a try, I stopped using fat emulsion.
On the fourth day, in the anxious waiting, the "alarm clock" didn’t ring.
After more than 20 days, the patient was transferred out of ICU, and the medical dispute with the patient’s family was resolved according to the "routine" at that time after several months.
Since then, the department has made a rule that in the acute stage of lung injury, fat emulsion is not applicable in principle.
If intravenous nutrition is needed, adopt "All in one" mode, and there is no special reason to prohibit intravenous fat emulsion alone.
Hemingway’s For Whom the Bell Tolls says: The bell ring for you!
As a doctor, always remember that the alarm bell rings for me. Medicine has made progress in the review, and the lessons brought by mistakes have benefited each of us for life in a sense more than the joy of success.
postscript
The lesson of this case:
After spinal cord shock, patients with cerebral infarction will basically have increased muscle tension on the affected side, from flaccid paralysis to hard paralysis. Increased tension of adductor muscles can easily lead to femoral head prolapse from joint capsule, which is a contraindication for femoral head replacement.
Pseudobulbar paralysis has a very high risk of aspiration, so try to avoid lying flat for a long time after operation. If necessary, consider lateral position, or reserve gastrointestinal decompression to prevent aspiration.
Intravenous nutrition should avoid single infusion of fat emulsion injection, and pay attention to avoid fat precipitation when using "All in one" mode three-liter bag to prepare nutrient solution, so as to avoid complications similar to fat embolism syndrome. Intravenous infusion of fat emulsion alone is prohibited. It is forbidden to add any electrolyte components. Pay attention to controlling the infusion speed and use central venous catheter as much as possible to prevent superficial phlebitis. Pay attention to check the patient’s fat clearance ability during the use of fat emulsion.
Low-dose hormone lung lavage combined with intravenous application of low-dose hormone may be effective for aspiration pneumonia.
The abnormal situation that patients appear repeatedly and regularly must pay attention to the investigation of iatrogenic factors.
This article starts: medical respiratory channel
Author: Bai Ding
Editor in charge: Dai Dai Zhang Li
Copyright statement
This article is original, welcome to forward the circle of friends.
– End –
Read the original text