Can’t high-flow humidified oxygen therapy through nose be used? Three guides teach you how to operate accurately
The original Xiaobu Medical Breathing Channel is included in the topic # Breathing Guide Interpretation of 6 Contents.
* For medical professionals only.

The latest expert consensus on clinical application of nasal high-flow oxygen therapy for emergency adults, an analysis!
Respiratory doctors should be familiar with nasal high-flow humidified oxygen therapy (HFNC). Since it was applied in mainland China in 2014, HFNC has been rapidly promoted and popularized in recent years, and its clinical effect is obvious to all.
Compared with traditional oxygen therapy (COT), noninvasive positive pressure ventilation (NPPV) and invasive positive pressure ventilation, HFNC has its unique advantages and certain limitations. In February, 2019, the Respiratory Critical Care Medicine Group of the Respiratory Branch of the Chinese Medical Association released the Expert Consensus on the Application of Clinical Norms of High-flow Humidified Oxygen Therapy for Adults (hereinafter referred to as the "Expert Consensus of 2019 Edition"), which gave everyone a comprehensive understanding of HFNC.
With the outbreak of COVID-19 epidemic, HFNC has also played an important role in the treatment of severe and critical COVID-19 patients. Therefore, the Respiratory Therapy Group of the Respiratory Branch of the Chinese Medical Association issued the Expert Consensus on the Use and Management of Nasal High-flux Oxygen Therapy for Patients in novel coronavirus [2] (hereinafter referred to as the Expert Consensus in 2020), which provided guidance for the use of HFNC in patients in COVID-19.
Of course, the clinical application of HFNC is not limited to respiratory patients, and any patient who needs aerobic treatment has potential indications for HFNC. Recently, the Emergency Medicine Branch of the Chinese Medical Association issued the Expert Consensus on Clinical Application of Nasal High-flux Oxygen Therapy for Emergency Adults [3] (hereinafter referred to as the Expert Consensus in 2021), focusing on the application of HFNC in emergency environment.
The guide is so spicy that I can’t read it. Today, the author will summarize and summarize the essence of these three guidelines, and show you what is unique about HFNC and how to use it in patients and emergency environment in COVID-19.
Let’s cut to the chase.
one
Basic concepts and principles of HFNC
In fact, nasal high-flow humidified oxygen therapy (HFNC) is well understood, which is a kind of treatment that can provide patients with high-flow inhaled gas with adjustable and relatively constant oxygen concentration, temperature and humidity through nasal congestion.
Compared with COT, HFNC highlights two advantages: high flow rate and heating and humidification. The common nasal tube has a small diameter, so it is difficult to achieve relatively constant high flow rate and oxygen concentration. However, HFNC can achieve these goals at the same time through high flow rate nasal plug and heating and humidification device.
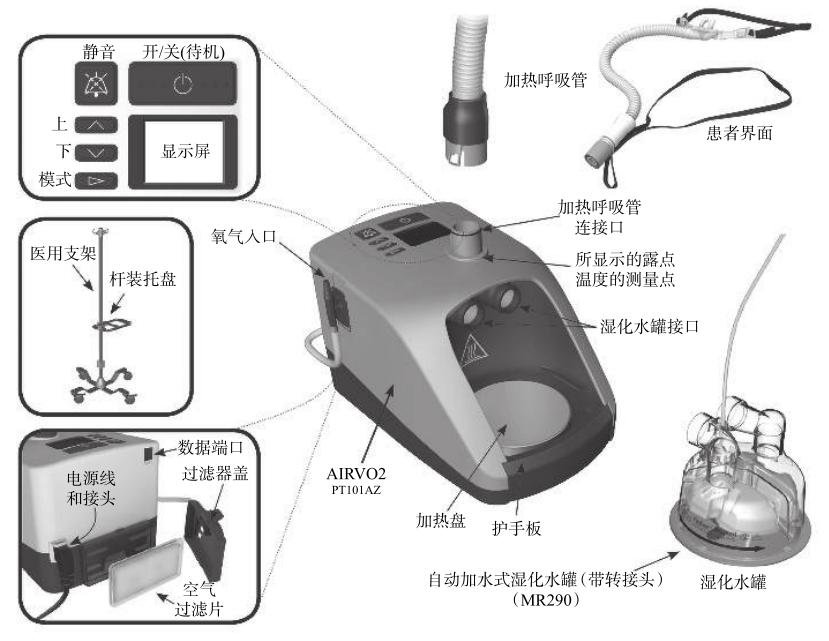
Figure 1 AIRVO2 HFNC
On this basis, HFNC can also achieve physiological effects similar to NPPV:
Positive End-expiratory Pressure (PEEP) effect: High-velocity gas can maintain a certain level of PEEP, which is beneficial to alveolar recruitment and qi-blood exchange at end-expiratory;
Physiological dead space scouring effect: high-velocity gas can also scour the gas left in the anatomically ineffective cavity of nasal cavity, oral cavity and pharynx at the end of expiration;
Maintain the function of mucociliary clearance system: relatively constant heating and humidifying gas can obviously reduce the dryness of nose, mouth and throat of patients, which is helpful to dilute sputum and expel phlegm;
Reduce the patient’s upper airway resistance and respiratory work: high-flow gas makes the patient not need to inhale hard, which can reduce the inspiratory resistance and reduce the patient’s respiratory work.
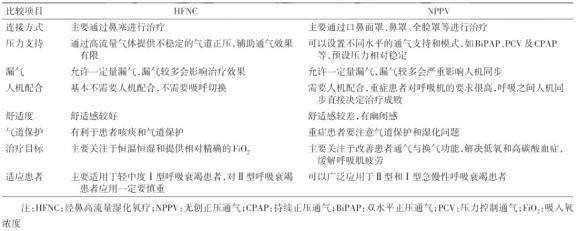
Of course, there are still some differences between HFNC and NPPV. The two oxygen therapy methods have their own advantages and are suitable for different patients and oxygen inhalation environments.
Table 1 Differences between HFNC and NPPV
2
Indications and contraindications of HFNC
As the saying goes, although something is good, it depends on whether it is useful or not. When to use it and when not to use it is a topic that everyone really cares about.
In fact, at present, there is no uniform standard for indications and contraindications of clinical application of HFNC. The indications of HFNC recommended by expert consensus in 2019 include:
Patients with mild or moderate hypoxemia (100 mmHg≤ PaO _ 2/fio _ 2 < 300 mmHg), no indication of emergency tracheal intubation and relatively stable vital signs;
Patients with mild ventilation dysfunction (pH≥7.3) can also be used cautiously, but they should be prepared to switch to NPPV or invasive positive pressure ventilation with tracheal intubation.
On this basis, the consensus of experts in the 2020 edition points out that it meets the diagnostic criteria of severe COVID-19 (respiratory distress, respiratory frequency ≥30 beats/min; At rest, oxygen saturation is ≤ 93%; Patients with PaO2/FiO2≤300mmHg) can consider using HFNC.
The 2021 edition of expert consensus did not specifically list the indications of HFNC, but recommended specific clinical scenarios:
Acute type I respiratory failure: using HFNC instead of COT to reduce the rate of tracheal intubation and the need for respiratory support upgrade; Patients who have received NPPV can try HFNC; under close monitoring if they are intolerant of NPPV.
Chronic obstructive pulmonary disease (COPD) with mild to moderate hypercapnia (pH > 7.25): HFNC can be used as one of the options for initial respiratory support; Patients who are intolerant of NPPV are advised to use HFNC;. HFNC; is not recommended for patients with pH < 7.25;
After extubation with mechanical ventilation: Patients who have been intubated for more than 24 hours and have high risk factors of respiratory failure after extubation should use HFNC instead of COT; after extubation; Patients with sequential NPPV after mechanical ventilation extubation should continue to use NPPV. If they are intolerant of NPPV, it is recommended to use HFNC;.
After surgery: High-risk and/or obese patients undergoing cardiac or thoracic surgery should use HFNC instead of COT immediately after surgery to reduce the need for re-intubation and respiratory support upgrade; Routine use of HFNC; is not recommended for patients after abdominal surgery.
Pre-oxygenation of tracheal intubation (providing oxygen to patients before tracheal intubation to maintain the stability of blood oxygen saturation during short-term asphyxia): HFNC; is not recommended for routine application during pre-oxygenation of tracheal intubation; Patients who have received HFNC before tracheal intubation can continue to use HFNC during preoxygenation and intubation.
Bronchoscopy: For patients without respiratory failure, HFNC should be used instead of COT to prevent hypoxemia during bronchoscopy; In patients with acute respiratory failure, HFNC can be used as a substitute for NPPV during bronchoscopy.
In addition, the 2021 edition of expert consensus also lists the application recommendations of HFNC in emergency special populations:
Immunosuppression: HFNC can be used as one of the initial oxygen therapy options for patients with immunosuppression complicated with acute type I respiratory failure. If patients who use NPPV are intolerant of NPPV, they can consider HFNC replacement therapy.
Heart failure: HFNC can be used as one of the initial oxygen therapy options for patients with heart failure, and patients who use NPPV can consider HFNC replacement therapy if they are intolerant;
Carbon monoxide poisoning: HFNC can be used as one of the initial oxygen therapy options for patients with mild carbon monoxide poisoning;
Palliative treatment: HFNC can be used as one of the initial oxygen therapy options for patients with palliative treatment, and patients with intolerance to NPPV can try HFNC.
Let’s talk about the contraindications of HFNC. In fact, the relevant contents of these three guides are similar. The contraindications mainly include:
Cardiac arrest;
Severe type I respiratory failure;
Moderate and severe respiratory acidosis hypercapnia (pH < 7.30);
Combined with multiple organ dysfunction.
three
Parameter setting of HFNC
After talking about indications and contraindications, let’s give you some dry goods and see how to set the parameters of HFNC. Compared with NPPV, HFNC needs to set fewer parameters, mainly including temperature, gas flow and oxygen concentration.
The setting range of temperature is generally 31~37℃, which is mainly adjusted according to the patient’s comfort and tolerance, and at the same time, a certain sputum viscosity is maintained, which makes the sputum easy to cough up.
The setting range of gas flow rate is generally 8-80L/min, and the highest oxygen concentration can reach 100%, which are mainly set according to the type of respiratory failure of patients:
Type I respiratory failure: the initial setting of gas flow rate is 30 ~ 40l/min; Titration of FIO _ 2 to maintain SpO2 _ 2 at 92%~96%, combined with dynamic adjustment of blood gas analysis, if the oxygenation target is not reached, the oxygen flow rate can be gradually increased to increase FIO _ 2 to 100% at the highest;
Type Ⅱ respiratory failure: the gas flow rate is initially set at 20~30 L/min, which is adjusted according to the patient’s tolerance and compliance. If CO2 retention is obvious, the flow rate can be set at 45~55 L/min or even higher, reaching the maximum flow rate that the patient can tolerate; Titrate FiO2 _ 2 to maintain the oxygen saturation (SpO2 _ 2) at 88%~92%, and dynamically adjust it with blood gas analysis.
To put it simply, the difference between type I respiratory failure and type II respiratory failure is that the former has no CO2 retention, and it is only necessary to adjust the oxygen concentration to achieve the oxygenation goal, while the latter has CO2 retention, so it is necessary to adjust the gas flow rate to achieve the goal of CO2 removal, and at the same time, it is necessary to adjust the oxygen concentration to maintain SpO2 in a relatively low constant range.
However, the use of HFNC does not mean that you can sit back and relax. It is necessary to closely monitor and identify patients who do not respond well to HFNC treatment as soon as possible to avoid delaying the upgrade of respiratory support and worsening the clinical prognosis. The consensus of experts in the 2021 edition points out that:
During the first 1-2 hours of HFNC, close observation should be made. If there are any failure prediction indicators (respiratory rate > 35 beats /min, SPO2≤88%, the ratio of SPO2/FiO2 to respiratory rate (ROX index) < 2.85, contradictory movements of chest and abdomen or use of auxiliary respiratory muscles, etc.), respiratory support should be upgraded in time (NPPV or invasive ventilation).
If the respiratory condition is still not improved after 48 hours of using HFNC, there are still any of the above predictors of failure, or the ROX index is gradually decreased, or the hemodynamics is unstable, it is regarded as a failure of HFNC treatment, and it is recommended to upgrade to invasive ventilation.
So when can the HFNC be removed? According to the consensus of experts in 2019, the parameters of HFNC will be gradually reduced after the primary disease is controlled. If the following criteria are met, the HFNC can be removed: inspiratory flow < <20L/min and fio2 < 30%.
On this basis, the 2021 edition of expert consensus recommended the specific process of evacuation of HFNC: during the evacuation of HFNC, it is suggested to reduce FiO2 first, and then reduce the gas flow rate. When the gas flow rate is reduced to 15L/min, stop using HFNC and change to COT.
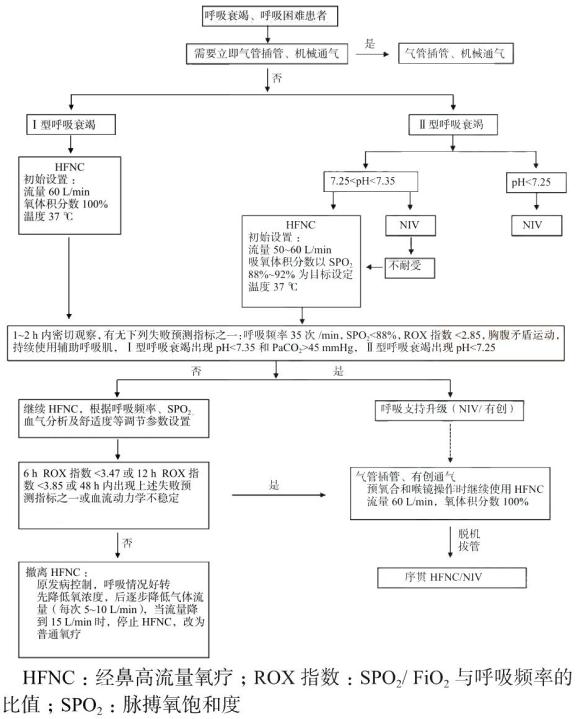
Fig. 2 Flow chart of HFNC usage
The above are the essence of the three HFNC guides. If you are interested, please read the original text, which contains more exciting contents!
Tips at the end of the article: forward this article to more people in need ~
References:
[1] Group of Respiratory Critical Care Medicine, Respiratory Branch of Chinese Medical Association, Working Committee of Critical Care Medicine, Respiratory Branch of Chinese Medical Association. Expert consensus on the application of clinical norms of high-flow humidified oxygen therapy for adults [J]. Chinese Journal of Tuberculosis and Respiratory Medicine, 2019,42(2):83-91.
[2] Ni Zhong, Qin Hao, Li Jie, et al. Expert consensus on the use and management of nasal high-flow oxygen therapy for novel coronavirus patients [J]. chinese journal of respiratory and critical care medicine, 2020,19(2):110-115.
[3] Emergency Physician Branch of Chinese Medical Association, Emergency Medicine Branch of Chinese Medical Association, China Emergency Medical Association, etc. Expert consensus on clinical application of nasal high-flow oxygen therapy for emergency adults [J]. chinese journal of critical care medicine, 2021,41(9):739-749.
This article starts: medical respiratory channel
Author: Xiao Bu
Editor in charge: Dai Dai Zhang Li
Copyright statement
Please contact authorization for the original reprint of this article.
– End –
Read the original text